Anti-inflammatory Targets for Hidradenitis Suppurativa Likely Vary by Patient
A better understanding of the pathophysiology of hidradenitis suppurativa (HS) has increased the number of inflammatory pathways known to drive its manifestations, which might make it possible to tailor therapies to the divergent phenotypes, according to two collaborating experts.
“We are seeing a role for many different inflammatory mechanisms, none of which consolidate into a single immunological pathway,” said James G. Krueger, MD, PhD, head of the Laboratory for Investigative Dermatology at The Rockefeller University in New York City.
Different inflammatory mechanisms explain various features and probably account for the inconsistent response to any single anti-inflammatory mechanism, Krueger noted. He described T- and B-cell activation with varying roles in different types of lesions during a presentation of his research on December 6 at the 28th Annual Mount Sinai Winter Symposium in New York City.
HS Treatment Predicted To Be Personalized
Recent research is leading to a growing array of treatments targeted at specific mediators or pathways of inflammation, but it appears these will not be interchangeable for different manifestations of disease, Krueger said.
Of the currently approved targeted therapies, such as the TNF inhibitor adalimumab, the interleukin (IL)-17A inhibitor secukinumab, and the IL-17A/F inhibitor bimekizumab, each has shown efficacy in many, but not all, patients, according to Krueger. The explanation appears to be that targeted cytokines and inflammatory pathways are more important for some types of activity, such as folliculitis, than others, such as fistulae.
For example, the treatment of draining tunnels has generally been less impressive with TNF inhibitors relative to drugs targeting IL-17F, Krueger noted. Although the IL-17 cytokine has proven to be an important target for psoriasis, he said it might be an even more important target for the fistula-dominant HS presentations.
The potential to select therapies for dominant disease pathways in HS is exciting because the pipeline of potential therapies for HS is substantial and includes a variety of drugs with novel mechanisms of action. Krueger described an “evolving HS treatment landscape” that includes drugs targeting IL-1-alpha/beta, JAK isoforms, IL-36, and Bruton tyrosine kinase (BTK) — an enzyme that plays an important role in B-cell signaling.
One advantage of drugs with new mechanisms of action is the role they can play in differentiating which inflammatory pathways drive which forms of HS pathology, Krueger said.
He provided several examples of treatments that have reached clinical testing. One, a dual-target agent called brivekimig, blocks both TNF and the OX40 ligand.
HS Might Involve Blocking Both T- and B-Cell Pathways
The mechanism of this benefit is still being evaluated, according to Krueger, but TNF inhibition is most closely associated with modification of B-cell-mediated inflammation, whereas inhibition of the OX40 ligand is associated with prevention of T-cell activation.
Many newer drugs, including brivekimig, are being evaluated in other inflammatory dermatologic diseases, such as atopic dermatitis. This presents new opportunities to compare and contrast drugs across specific types of anti-inflammatory activity.
As another example, remibrutinib, a BTK inhibitor, also met the primary endpoint for improvement in HiSCR50 in a placebo-controlled phase 2b trial. For the two tested doses, a greater response was observed with the higher dose for both the primary endpoint of HiSCR50 and the secondary endpoint of draining tunnels.
Krueger pointed out that the anti-inflammatory effect of BTK inhibition is attributed to the prevention of B-cell activation and said there is growing interest in determining how inhibition of B- and T-cell activity compares in HS.
The benefit from diverse targets along the inflammatory pathway suggests “it might make sense to target inflammation more broadly” by using drugs affecting multiple inflammatory pathways, but Krueger suggested that developing drugs to treat specific disease manifestations is now looking more promising than searching for one drug that by itself controls HS.
This principle is now a major direction of research, according to Kristina Navrazhina, MD, PhD, who is completing her training in dermatology at the Icahn School of Medicine at Mount Sinai in New York City. Navrazhina, whose PhD was based on HS research, published several papers on this disease before starting her residency.
In treating the disease rather than the phenotype, “we have been throwing whatever is approved or covered at HS without understanding the target,” she said in a separate presentation at the Mount Sinai symposium. “This often means years of ineffectual therapy.”
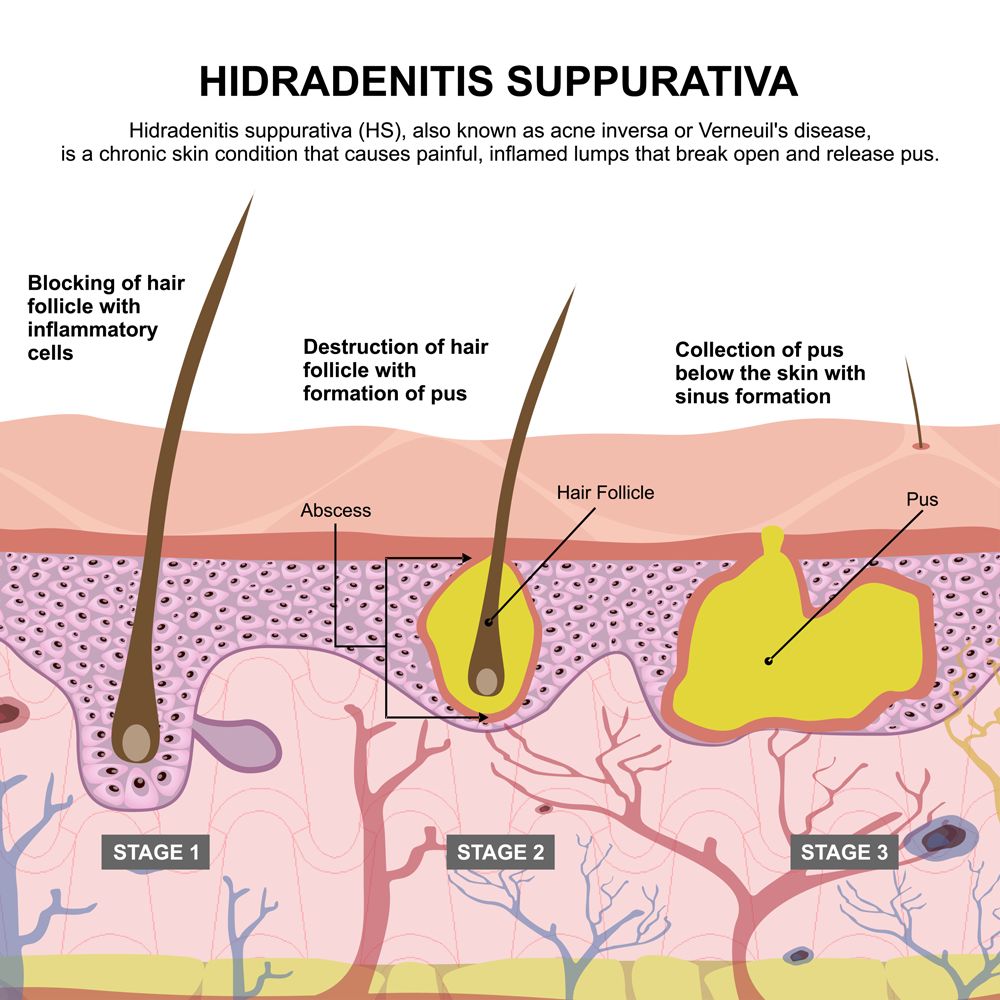
“It was not that long ago that we thought HS was a disease of follicular occlusion, but we now appreciate that it is a systemic disease,” she said. Often, an HS nodule “is just the tip of the iceberg.”
Lately, Navrazhina has been looking at tape strips as a minimally invasive means of RNA sequencing to identify lesions with a phenotypic profile. However, citing the long average diagnostic delay for HS, she is also pursuing approaches to diagnose HS earlier and move quickly to highly effective therapy, even when clinical signs of disease appear mild.
“Why is HS so hard to clear? We are probably missing the window of opportunity. By the time we make the diagnosis and start treatment, the inflammatory burden is so high that it is not surprising that the efficacy of biologics has been limited,” she said.
She expressed concern about focusing only on visible lesions, citing studies in which biopsies taken 10 cm from lesional skin suggest a high degree of ongoing inflammation on the basis of biomarkers. She said fistulae under the skin often are already forming when skin involvement is still mild.
The recent interest in HS reflects the appreciation of the systemic nature and the complex network of inflammatory pathways, increasing the number of additional potential targets for treatment. This will drive clinical management to personalized therapy, she predicted.
Even in patients with mild disease, “we need to be thinking beyond nodules,” she said.
Write a public review