Dec,2025

Vitamin B6 Pills Tied to Neuropathy: Stricter Rules Urged
30-12-2025Australia will significantly tighten the regulation of dietary supplements with vitamin B6 (pyridoxine) starting in 2027, under a reclassification by the Therapeutic Goods Administration. Products with more than 50 mg of vitamin B6 will then be available only in pharmacies, and those with more than 200 mg will require a prescription. The move follows numerous reports of sometimes severe sensorimotor polyneuropathies after long-term high-dose supplementation.
Concerns are also growing in Germany that B6 supplements are underestimated. “A restriction of over-the-counter [OTC] availability would be desirable here as well,” said Hans-Jürgen Gdynia, chief of neurology at m&i Fachklinik Enzensberg, a specialist clinic and rehabilitation center located in Füssen, Germany. Preparations with B vitamins are “advertised in pharmacies, on television, and online as beneficial for the nerves.” The problem, he said, is that many people “equate over-the-counter with harmless.” That belief is deceptive.
The German Federal Institute for Risk Assessment (BfR) has recommended since last year that adults and adolescents aged 15 years or older should not consume more than 0.9 mg of vitamin B6 per day from supplements. The European Food Safety Authority (EFSA) in 2023 lowered the tolerable total daily intake for adults from 25 mg/d to 12 mg/d. Amounts above that are considered unsafe. For children, upper limits range from 2 mg/d to 11 mg/d depending on body weight.
High-Dose Products Still Sold OTC
Despite these very low recommendations, the German market still offers numerous products with 25-50 mg of vitamin B6 per capsule or tablet, both as single-ingredient products and as part of high-dose B-complex vitamins. Investigation of supplements for toddlers and preschoolers, as well as earlier analysis of sports supplements sold online, shows that some products contain vitamin B6 levels that exceed age-appropriate reference values or the presumed safe upper limits many times over.
How many people actually take such products long-term is unknown. Studies usually assess overall supplement use rather than targeted B6 supplementation. Clinicians observe, however, that many patients combine multiple products and thereby unknowingly reach high total doses.
B6-Associated Polyneuropathies
That high B6 intake can be neurotoxic has been known for decades. As early as 1983, a team in The New England Journal of Medicine reported sensory neuropathy from chronic high-dose pyridoxine use, with symptoms often improving after the supplement was stopped.
What is new is how often such cases now occur. At this year’s German Society for Neurology congress, Gdynia and colleagues presented a case series of eight patients who developed polyneuropathy due to B6 hypervitaminosis. “And these are only patients who presented to our neurology clinic over 4 years,” he emphasized. “So it’s not as rare as you think.”
The affected individuals had taken OTC products — mostly B-complex vitamins, often for “general strengthening,” in some cases on a physician’s recommendation. “Extremely high-dose preparations aren’t even necessary. The hypervitaminosis in all cases arose from products bought at a pharmacy or drugstore,” Gdynia said.
Include B6 in Routine Workup
Given this clustering, Gdynia calls for changes in diagnostic practice. “In polyneuropathy, you should always check the B6 level,” he said. Many cases are overlooked because histories do not specifically ask about supplements, and B6 is often not measured in unclear neuropathies.
In his view, this diagnostic gap should be reflected in the guideline “Diagnostics in polyneuropathies” of the German Society for Neurology, which currently recommends measuring vitamin B6 only in certain cases, not generally. “This belongs in routine diagnostics,” he emphasized. The reason: B6-induced neuropathy is potentially reversible. “After stopping the preparation, many cases improve gradually, provided the damage has not lasted too long.”
Moderate Long-Term Doses Can Harm
In Australia, approximately 250 cases of B6-induced polyneuropathy were reported before the regulatory decision. The majority involved people who had taken 100-200 mg/d or more over extended periods.
At very high doses, a polyneuropathy can occur in about 1%-4% of those chronically exposed, still rare but by no means negligible, said Peter Crack, a neuropharmacologist at The University of Melbourne, Melbourne, Australia, in comments to the Australian Science Media Centre. “Even moderate but sustained intakes (eg, 50 mg/d over months to years) have been linked to sensory neuropathy in susceptible individuals.”
“Neuropathy is rarely seen with dietary intake alone and occurs almost exclusively in people taking supplements at doses well above physiological needs,” Crack emphasized.
Water-Soluble Vitamin Myth
It is widely believed that water-soluble vitamins are harmless because excess amounts are excreted. “I also learned in medical school that only fat-soluble vitamins are stored and can be dangerous,” Gdynia said. “But too much vitamin B6 can obviously cause significant harm in the body.”
Awareness of hypervitaminosis is “not sufficiently developed in either the general population or the medical community.” Patients rarely volunteer information about self-purchased supplements, and physicians often do not specifically ask about supplements in the workup of polyneuropathies.
Stricter Rules Needed
Following the new EFSA assessment, the BfR proposed in 2024 that supplements for adults contain no more than 0.9 mg of vitamin B6 per daily dose. Even stricter limits apply for children. However, these values are not legally binding. That explains why products with 20-50 times higher contents are still available in drugstores and online shops.
Gdynia, therefore, advocates for clearer regulation, similar to that in Australia. “The dangers posed by hypervitaminosis are not sufficiently highlighted. We need more education and stricter rules.”
Dec,2025
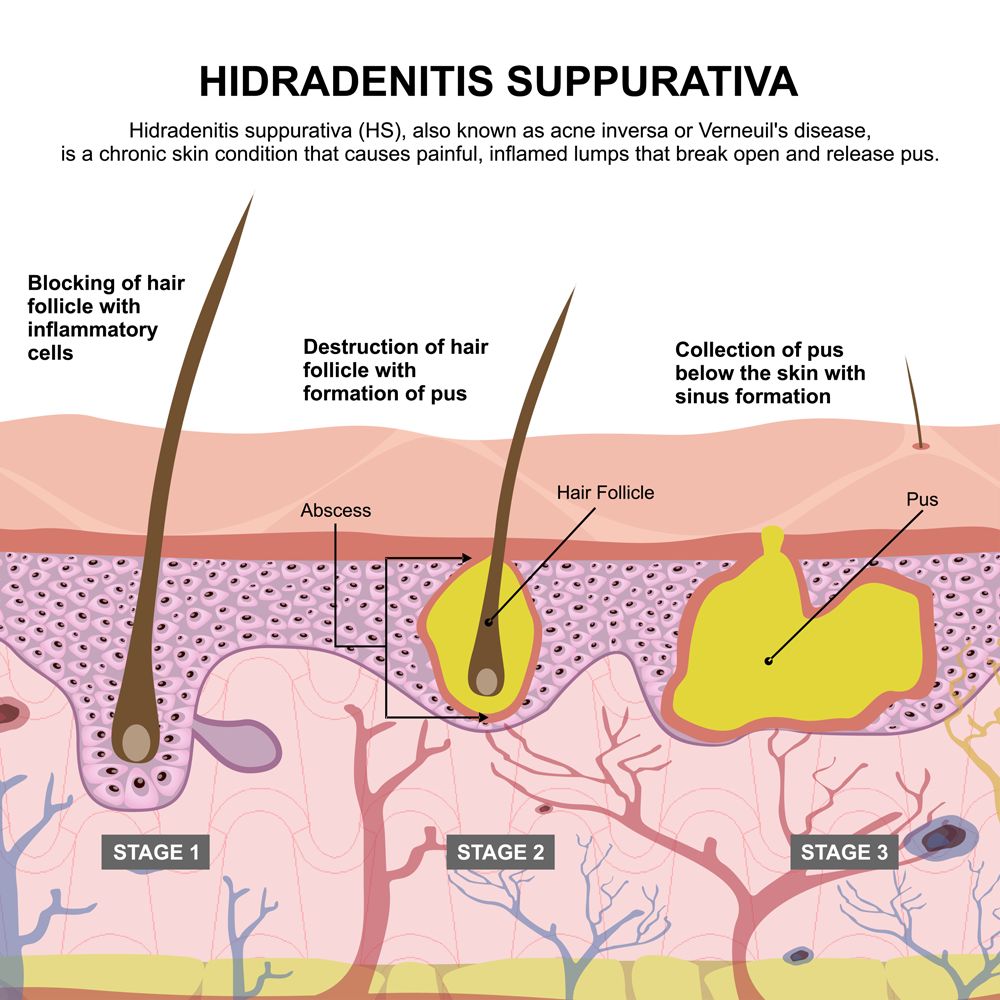
Anti-inflammatory Targets for Hidradenitis Suppurativa Likely Vary by Patient
31-12-2025A better understanding of the pathophysiology of hidradenitis suppurativa (HS) has increased the number of inflammatory pathways known to drive its manifestations, which might make it possible to tailor therapies to the divergent phenotypes, according to two collaborating experts.
“We are seeing a role for many different inflammatory mechanisms, none of which consolidate into a single immunological pathway,” said James G. Krueger, MD, PhD, head of the Laboratory for Investigative Dermatology at The Rockefeller University in New York City.
Different inflammatory mechanisms explain various features and probably account for the inconsistent response to any single anti-inflammatory mechanism, Krueger noted. He described T- and B-cell activation with varying roles in different types of lesions during a presentation of his research on December 6 at the 28th Annual Mount Sinai Winter Symposium in New York City.
HS Treatment Predicted To Be Personalized
Recent research is leading to a growing array of treatments targeted at specific mediators or pathways of inflammation, but it appears these will not be interchangeable for different manifestations of disease, Krueger said.
Of the currently approved targeted therapies, such as the TNF inhibitor adalimumab, the interleukin (IL)-17A inhibitor secukinumab, and the IL-17A/F inhibitor bimekizumab, each has shown efficacy in many, but not all, patients, according to Krueger. The explanation appears to be that targeted cytokines and inflammatory pathways are more important for some types of activity, such as folliculitis, than others, such as fistulae.
For example, the treatment of draining tunnels has generally been less impressive with TNF inhibitors relative to drugs targeting IL-17F, Krueger noted. Although the IL-17 cytokine has proven to be an important target for psoriasis, he said it might be an even more important target for the fistula-dominant HS presentations.
The potential to select therapies for dominant disease pathways in HS is exciting because the pipeline of potential therapies for HS is substantial and includes a variety of drugs with novel mechanisms of action. Krueger described an “evolving HS treatment landscape” that includes drugs targeting IL-1-alpha/beta, JAK isoforms, IL-36, and Bruton tyrosine kinase (BTK) — an enzyme that plays an important role in B-cell signaling.
One advantage of drugs with new mechanisms of action is the role they can play in differentiating which inflammatory pathways drive which forms of HS pathology, Krueger said.
He provided several examples of treatments that have reached clinical testing. One, a dual-target agent called brivekimig, blocks both TNF and the OX40 ligand.
HS Might Involve Blocking Both T- and B-Cell Pathways
The mechanism of this benefit is still being evaluated, according to Krueger, but TNF inhibition is most closely associated with modification of B-cell-mediated inflammation, whereas inhibition of the OX40 ligand is associated with prevention of T-cell activation.
Many newer drugs, including brivekimig, are being evaluated in other inflammatory dermatologic diseases, such as atopic dermatitis. This presents new opportunities to compare and contrast drugs across specific types of anti-inflammatory activity.
As another example, remibrutinib, a BTK inhibitor, also met the primary endpoint for improvement in HiSCR50 in a placebo-controlled phase 2b trial. For the two tested doses, a greater response was observed with the higher dose for both the primary endpoint of HiSCR50 and the secondary endpoint of draining tunnels.
Krueger pointed out that the anti-inflammatory effect of BTK inhibition is attributed to the prevention of B-cell activation and said there is growing interest in determining how inhibition of B- and T-cell activity compares in HS.
The benefit from diverse targets along the inflammatory pathway suggests “it might make sense to target inflammation more broadly” by using drugs affecting multiple inflammatory pathways, but Krueger suggested that developing drugs to treat specific disease manifestations is now looking more promising than searching for one drug that by itself controls HS.
This principle is now a major direction of research, according to Kristina Navrazhina, MD, PhD, who is completing her training in dermatology at the Icahn School of Medicine at Mount Sinai in New York City. Navrazhina, whose PhD was based on HS research, published several papers on this disease before starting her residency.
In treating the disease rather than the phenotype, “we have been throwing whatever is approved or covered at HS without understanding the target,” she said in a separate presentation at the Mount Sinai symposium. “This often means years of ineffectual therapy.”
“It was not that long ago that we thought HS was a disease of follicular occlusion, but we now appreciate that it is a systemic disease,” she said. Often, an HS nodule “is just the tip of the iceberg.”
Lately, Navrazhina has been looking at tape strips as a minimally invasive means of RNA sequencing to identify lesions with a phenotypic profile. However, citing the long average diagnostic delay for HS, she is also pursuing approaches to diagnose HS earlier and move quickly to highly effective therapy, even when clinical signs of disease appear mild.
“Why is HS so hard to clear? We are probably missing the window of opportunity. By the time we make the diagnosis and start treatment, the inflammatory burden is so high that it is not surprising that the efficacy of biologics has been limited,” she said.
She expressed concern about focusing only on visible lesions, citing studies in which biopsies taken 10 cm from lesional skin suggest a high degree of ongoing inflammation on the basis of biomarkers. She said fistulae under the skin often are already forming when skin involvement is still mild.
The recent interest in HS reflects the appreciation of the systemic nature and the complex network of inflammatory pathways, increasing the number of additional potential targets for treatment. This will drive clinical management to personalized therapy, she predicted.
Even in patients with mild disease, “we need to be thinking beyond nodules,” she said.
Jan,2026
Maintaining a healthy weight may help avoid low back pain
06-01-2026Low back pain (LBP) is a prevalent condition associated with disability, work loss, and economic burden to healthcare. Significant risk factors include poor sleep, physical and psychological stress, inactivity, advanced age, and smoking. The contribution of greater weight and body mass index (BMI) to the risk of LBP is less clear. Many past clinical studies have been small (fewer than 1,000 patients) or in specific patient groups, such as young men or patients who come to a subspecialty pain clinic, making those results more specific to those populations.
In a new study from Boston University Chobanian & Avedisian School of Medicine, researchers have found that individuals who are overweight or obese have a significantly higher risk of developing LBP compared to those with a normal BMI.
Low back pain is one of the most common complaints patients have for their medical providers. While medications, formal physical therapy, and other treatments can help, correcting risk factors, such as smoking or deconditioning, also helps LBP. The current study suggests that weight control and maintaining a lower BMI in the healthy range can be beneficial for LBP symptoms as well."
Michael D. Perloff, MD, PhD, corresponding author, assistant professor of neurology, Boston University Chobanian & Avedisian School of Medicine
Using computer analysis, the researchers reviewed the medical records of more than 110,000 patients, 18 years or older, who had visited an urban teaching hospital for outpatient care over the course of one year. Patient demographics, including age, sex at birth, height, weight, BMI, and whether a complaint of low back pain was reported at the visit was recorded.
The researchers found the prevalence of patients reporting low back pain increased with weight from a low healthy weight or BMI of 18 (or 90 pounds) up to an obese weight of BMI 35 (or 240 pounds). For BMIs beyond 35, the prevalence of low back pain did not continue to increase but stayed the same. For the range of 18-35 BMI, researchers found that for every increased unit of BMI (or 10 pounds), the prevalence of low back pain increased by 7%.
While not everyone with a higher BMI will experience back pain, the researchers documented the increased risk of it occurring. "Our study strongly suggests that maintaining a healthy weight or BMI is likely helpful at avoiding low back pain," adds Perloff, who is also director of pain medicine at Boston Medical Center.
These findings appear online in the journal Pain Medicine.
Perloff, M. D., et al. (2025). Body Mass Index and Prevalence of Low Back Pain: Correlation in a Large, Contemporary Cohort. Pain Medicine. doi: 10.1093/pm/pnaf178. https://academic.oup.com/painmedicine/advance-article-abstract/doi/10.1093/pm/pnaf178/8384258?redirectedFrom=fulltext
Jan,2026
Drug Shortages Stress Primary Care
13-01-2026Drug shortages in the United States have prompted 87% of clinicians to make changes in their practice, according to data from a new survey of approximately 900 individuals.
Persistent drug shortages arise from multiple factors, including supply chain disruptions, a limited number of manufacturers, regulatory burdens, small profit margins, as well as external factors such as natural disasters and unforeseen surges in demand for certain drugs. However, data on the effect of drug shortages on clinical practice are limited, wrote Jennie B. Jarrett, PharmD, director of science and drug policy at the American Medical Association (AMA) in Chicago, and colleagues.
In a study published in JAMA Network Open, the researchers investigated the effect of drug shortages on primary care clinicians and their patients via a cross-sectional, web-based survey conducted from July 2024 to August 2024. The final analysis included 902 primary care clinicians from a combination of family medicine practices (42%), outpatient-only practices (75%), urban settings (78%), and private practices (71%). Of these, 795 reported a perceived drug shortage in the past 6 months.
Respondents reported that drug shortages affected 20% of their patients on average. Overall, endocrinology drugs had the highest rate of severe outcomes associated with shortages (54%), followed by stimulants (52%), drugs for infectious diseases (26%), pulmonology (17%), and pain management (14%). Pediatricians reported the greatest impact from shortages associated with infectious disease, pulmonology, and stimulant medications.
Among the 87% of clinicians who reported changes in quality of care based on shortages, 92% said they changed the medication of choice, while 63% said they postponed prescribing. Pediatricians were less likely to postpone prescribing than family medicine physicians or internal medicine physicians.
The top considerations in drug shortage management were drug efficacy (89%), adverse effects (81%), out-of-pocket costs (78%), prior authorization (73%), and route of administration (58%). The most commonly reported outcome of a drug shortage was discontinuation of the medication (98%). However, approximately half (49%) reported disease progression, 13% reported major adverse events, and 2% reported patient deaths.
In addition, 44% of respondents reported concerns that no substitute drug might be available, 241 (30%) described requiring a combination of substitute medications to manage a shortage, and 85 (11%) were concerned about dispensing errors from changing treatment.
Notably, the findings highlight the lack of communication on drug shortages, the researchers wrote in their discussion. Patient communication and community pharmacists were the most common sources of drug shortage notification (73% and 70%, respectively), and resolution of a shortage (61% and 57%, respectively).
The findings were limited by several factors, including the overestimation of perceived drug shortages because of oversampling of physicians who were affected, possible lack of disclosure of outcomes by patients and physicians, and the inability to prove that responses were caused by genuine drug shortages, the researchers wrote.
Although some of the outcomes of shortages, such as discontinuing unavailable medications, were not unexpected, the severity of outcomes reported by physicians, including major adverse events and death, was surprising, Jarrett told Medscape Medical News. The survey findings also highlight the administrative burden of drug shortages on primary care clinicians, she added.
The survey’s main takeaway is that physician-led, team-based care is important for managing challenges posed by drug shortages and improving access to medications, Jarrett said. “Communication and care coordination of physicians and pharmacists are integral to individualized, patient-centered care,” she added.
However, the results suggest the need for better communication and strategies to manage the reported administrative burdens accompanying drug shortages. These burdens included prior authorization, frustration, and burnout, and respondents reported a median of 0.5 full-time equivalents of new staff time to manage the added workload associated with drug shortage, she said.
In addition, given the reported lack of physician awareness of drug shortages, physician perceptions of what is and is not available at any given time may differ from the actual supply, Jarrett said. “Similarly, the gap in awareness of when a drug has its shortage resolved compared to when it is ongoing may cause physicians to alter their practice longer than necessary,” she said.
Confusion in the Clinic
Medical breakthroughs in diagnosing, treating, and preventing diseases do not have real-world meaning unless they are getting to the patients, said Tim Joos, MD, an internist and pediatrician at Neighborcare Health in Seattle. “This is never more obvious than when a therapy that a patient has been benefiting from is interrupted by problems with short supply and delivery logistics,” said Joos, who was not involved in the study.
Analysis of the causes and effects of these interruptions is important to improve healthcare and overall public health, Joos told Medscape Medical News. “The study highlights a lot of what I see in my own practice,” he said. Direct communication from pharmacies to prescribers about a drug shortage is rare, he said. “The patients themselves are often confused about why they didn’t get the medicine, and I often don’t hear about it until months later when they come in for follow-up and don’t have the medicine,” he said. Even then, the reason for the shortage, whether a supply issue or formulary issue, is often unclear, he added.
“Improved communication about shortages by pharmacies, pharmaceutical and insurance companies, and perhaps health departments would help mitigate the detrimental effects of drug shortages,” Joos said.
The study received no outside funding. Jarrett disclosed grants from the CDC unrelated to the current study. Jarrett’s opinions are her own and do not reflect any AMA policy. Joos disclosed no financial conflicts of interest.
Jan,2026
Newly Discovered Immune 'Traffic Controller' Can Be Hijacked By Cytomegalovirus
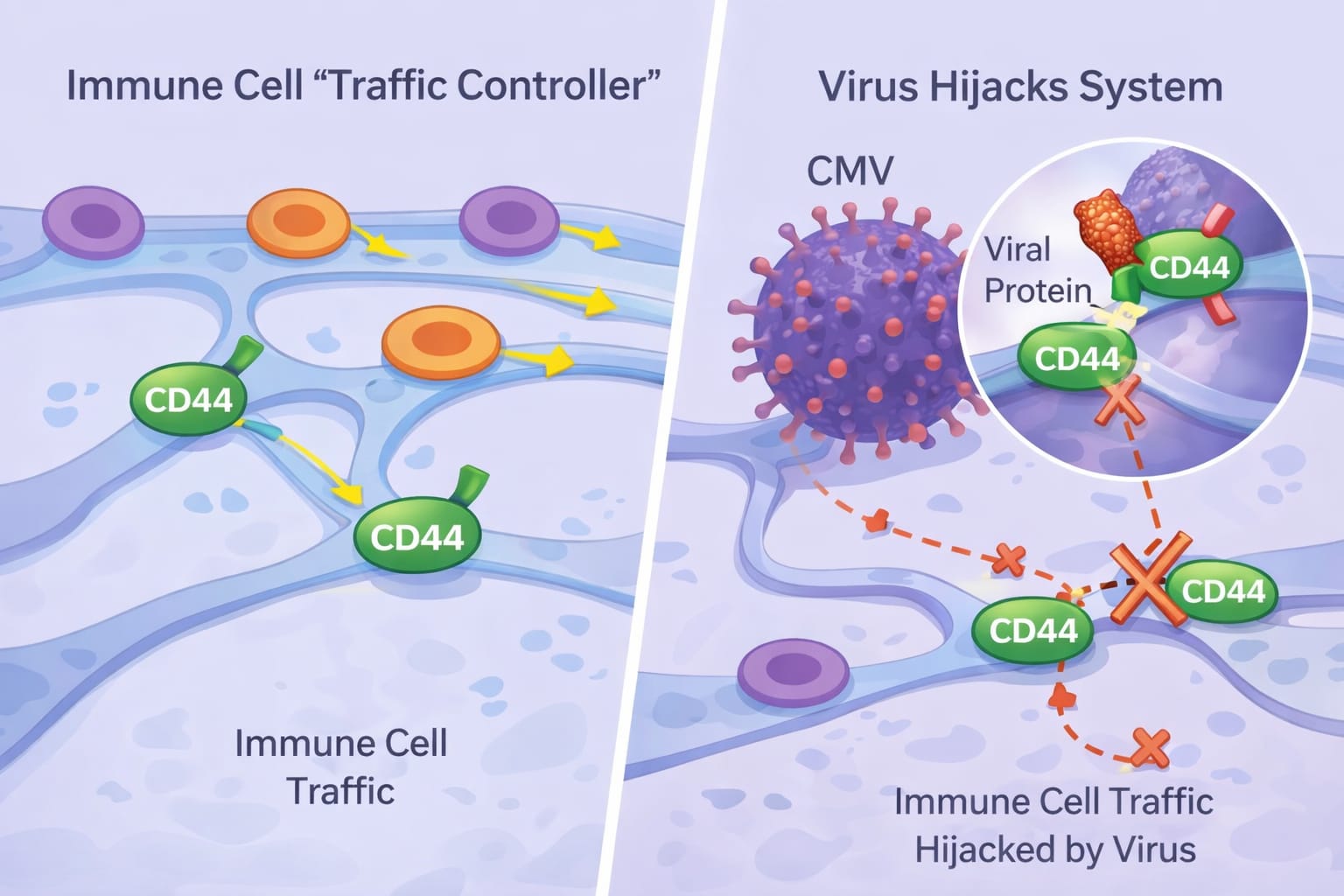
26-01-2026Researchers from Monash University and the Lions Eye Institute have discovered a tissue protein that acts as a central 'traffic controller' for immune cells and can be hijacked by a virus to weaken immune responses.
Published in Nature, the study discovered a key mechanism that controls how immune cells coordinate their responses, and how a common virus can sabotage it.
The research reveals that a molecule called CD44 centrally controls the network of support cells that guide immune system function.
Within this network of support cells, stromal cells help immune cells move efficiently and exchange the information needed to fight infections, respond to vaccines, and maintain overall health.
The research team discovered that cytomegalovirus (CMV) can hijack this system by producing a protein that blocks CD44 function on stromal cells, derailing immune cell traffic at its source and weakening the body's antiviral response.
Lead researcher Professor Mariapia Degli-Esposti, Head of Experimental and Viral Immunology at Monash Biomedicine Discovery Institute and Head of Experimental Immunology at the Lions Eye Institute, said the findings fundamentally change how scientists understand the signals that shape immune function.
"Think of the immune system like a busy city with millions of cells patrolling to keep us safe," Professor Degli-Esposti said.
"CD44 acts as the central traffic controller; it keeps immune cells moving and coordinates their interactions at the right place and time.
"Our study identifies CD44 as a master regulator of immune cell movement and communication and shows that viruses can undermine immunity not only by attacking immune cells directly, but also by targeting the essential tissue infrastructure they rely on.
"This is a completely new way for a virus to target an immune response."
Co-lead researcher Dr. Chris Andoniou, a Senior Research Fellow at Monash Biomedicine Discovery Institute and at the Lions Eye Institute, said the findings have wide-ranging implications for human health.
"Because CD44 plays such a central role in regulating immune activity, drugs inspired by the viral protein identified in this study could be developed to precisely dampen harmful inflammation," Dr. Andoniou said.
"By learning from the virus, we may be able to design therapeutic molecules that safely reduce excessive immune activation, which could ultimately help manage and treat autoimmune conditions.
"We are still in the early stages, but this is an exciting development."
Write a public review